Heart disease is a leading cause of death worldwide and it's vital that we understand the factors that can increase or decrease our risk of developing it. Recently, a study titled "Comparison of Seven Popular Structured Dietary Programs and Risk of Mortality and Major Cardiovascular Events in Patients at Increased Cardiovascular Risk: Systematic Review and Network Meta-Analysis" was conducted to determine the effectiveness of structured dietary and health behavior programs in preventing mortality and major cardiovascular events in patients at increased risk of cardiovascular disease.
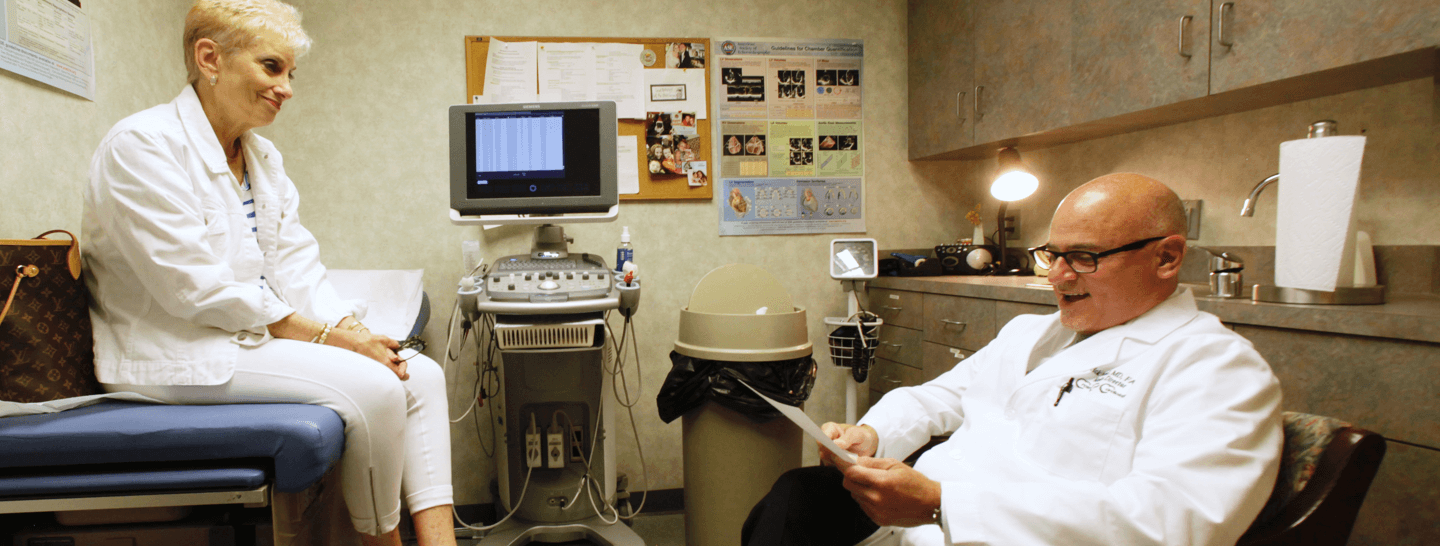
At Cross County Cardiology, we believe it's essential to share this data with our community. By understanding which dietary programs can help prevent heart disease and death, patients can make more informed decisions about their health and lifestyle choices. We want to empower our community to prioritize heart health by making informed choices and seeking professional guidance.
The study highlighted the importance of a healthy diet, exercise, and other healthy habits in reducing the risk of heart disease and related events. It found that structured dietary programs can significantly reduce the risk of all-cause mortality and non-fatal myocardial infarction in patients at increased cardiovascular risk. In particular, Mediterranean and low-fat diets were found to be effective in reducing the risk of heart disease and stroke.
At Cross County Cardiology, we strongly recommend a heart-healthy lifestyle that includes a healthy diet, regular exercise, and other healthy habits. By prioritizing heart health, patients can significantly reduce their risk of heart disease and related events.
We also recommend that patients seek professional guidance when making changes to their diet and lifestyle. Our team of experienced cardiologists and nutritionists can provide personalized recommendations to help our patients reduce their risk of heart disease and related events.
In conclusion, we believe that sharing this data with our community is an essential step in improving heart health and reducing the risk of heart disease and related events. At Cross County Cardiology, we are committed to providing our patients with the tools and resources they need to lead a heart-healthy lifestyle.
Read the study by clicking here.