Understanding the distinction between a heart attack and sudden cardiac death is crucial for effective cardiovascular health management. In this blog, we explore the key differences and their implications, aiming to provide you with vital information that could potentially save lives.
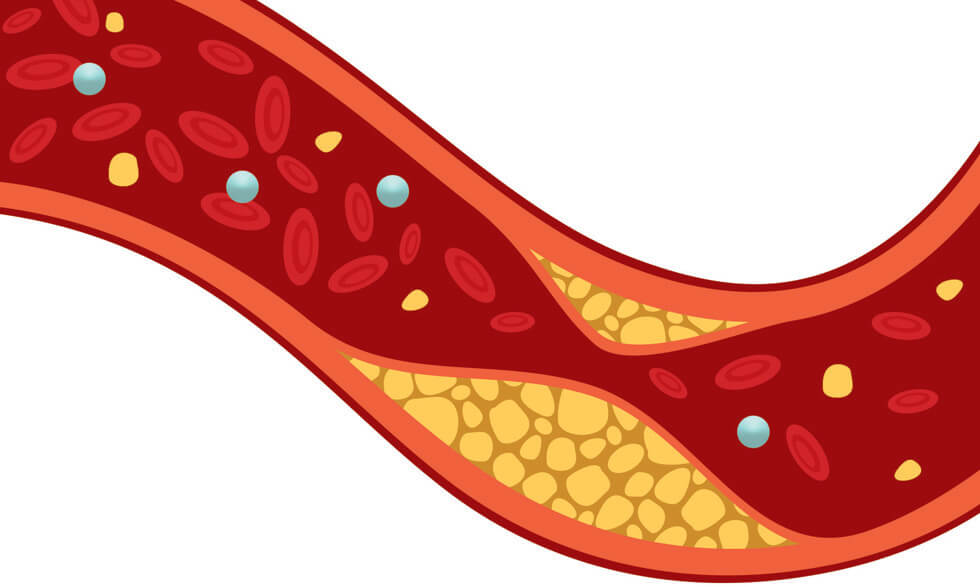
Previous studies have shown reduced cardiovascular risk with increasing high-density lipoprotein cholesterol (HDL-C) levels. However, recent data in the general population have shown increased risk of adverse outcomes at very high concentrations of HDL-C. Thus, we aimed to study the gender-specific relation between very high HDL-C levels (>80, >100 mg/100 ml) and adverse cardiovascular outcomes and the genetic basis in the general population enrolled in the United Kingdom Biobank.
A total of 415,416 participants enrolled in the United Kingdom Biobank without coronary artery disease were included in this prospective cohort study, with a median follow-up of 9 years.
A high HDL-C level >80 mg/100 ml was associated with increased risk of all-cause death (Hazard ratio [HR] 1.11, confidence interval [CI] 1.03 to 1.20, p = 0.005) and cardiovascular death (HR 1.24, CI 1.05 to 1.46, p = 0.01) after adjustment for age, gender, race, body mass index, hypertension, smoking, triglycerides, LDL-C, stroke history, heart attack history, diabetes, eGFR, and frequent alcohol use (defined as ≥3 times/week) using Cox proportional hazard and Fine and Gray's subdistribution hazard models, respectively.
In gender-stratified analyses, such associations were only observed in men (all-cause death HR 1.79, CI 1.59 to 2.02, p <0.0001; cardiovascular death HR 1.92, CI 1.52 to 2.42, p <0.0001), but not in women (all-cause death HR 0.97, CI 0.88 to 1.06, p = 0.50; cardiovascular death HR 1.04, CI 0.83 to 1.31, p = 0.70). The findings persisted after adjusting for the genetic risk score comprised of known HDL-C–associated single nucleotide polymorphisms.
Very high HDL-C levels are associated with an increased risk of all-cause death and cardiovascular death among men but not in women in the general population free of coronary artery disease.
-
At Cross County Cardiology, we care about you and helping you prevent cardiovascular issues and deaths. This is why we recommend annual checkups with one of our skilled and knowledgable doctors. Make an appointment today by calling 201-776-8690 or go online, it could just save your life!